What is restless legs syndrome?
Restless legs syndrome (RLS), also called Willis-Ekbom Disease, causes unpleasant or uncomfortable sensations in the legs and an irresistible urge to move them. Symptoms commonly occur in the late afternoon or evening hours, and are often most severe at night when a person is resting, such as sitting or lying in bed.
They also may occur when someone is inactive and sitting for extended periods (for example, when taking a trip by plane or watching a movie). Since symptoms can increase in severity during the night, it could become difficult to fall asleep or return to sleep after waking up. Moving the legs or walking typically relieves the discomfort but the sensations often recur once the movement stops.
RLS is classified as a sleep disorder since the symptoms are triggered by resting and attempting to sleep, and as a movement disorder, since people are forced to move their legs in order to relieve symptoms. It is, however, best characterized as a neurological sensory disorder with symptoms that are produced from within the brain itself.
RLS is one of several disorders that can cause exhaustion and daytime sleepiness, which can strongly affect mood, concentration, job and school performance, and personal relationships. Many people with RLS report they are often unable to concentrate, have impaired memory, or fail to accomplish daily tasks. Untreated moderate to severe RLS can lead to about a 20 percent decrease in work productivity and can contribute to depression and anxiety. It also can make traveling difficult.
It is estimated that up to 7-10 percent of the U.S. population may have RLS. RLS occurs in both men and women, although women are more likely to have it than men. It may begin at any age. Many individuals who are severely affected are middle-aged or older, and the symptoms typically become more frequent and last longer with age.
More than 80 percent of people with RLS also experience periodic limb movement of sleep (PLMS). PLMS is characterized by involuntary leg (and sometimes arm) twitching or jerking movements during sleep that typically occur every 15 to 40 seconds, sometimes throughout the night. Although many individuals with RLS also develop PLMS, most people with PLMS do not experience RLS.
Fortunately, most cases of RLS can be treated with non-drug therapies and if necessary, medications.
Gabapentin in the management of restless legs syndrome (RLS) has been evaluated in small controlled trials, demonstrating benefits compared with placebo. Gabapentin enacarbil is FDA-approved for the treatment of RLS .

The American Academy of Sleep Medicine (AASM) guidelines regarding RLS management consider gabapentin effective based on low-level evidence and note that patients with pain symptoms appeared to benefit most.
The benefit-risk ratio is unclear. The European Federation of Neurological Societies/European Neurological Society/European Sleep Research Society (EFNS/ENS/ESRS) Task Force guidelines consider gabapentin effective for short-term management and possibly effective for long-term management of RLS.
Additional study is needed to establish optimal dosing. Based on the International Restless Legs Syndrome Study Group, European Restless Legs Syndrome Study Group, and RLS Foundation (IRLSSG/EURLSSG/RLS-F) guidelines for the prevention and treatment of dopaminergic augmentation in restless legs syndrome, α2δ ligands (eg, gabapentin) are effective and should be considered for the initial treatment of patients with RLS due to their minimal risk of augmentation.
Additionally, patients who experience augmentation on dopaminergic agents may benefit from a switch to α2δ ligands (eg, gabapentin). However, the guidelines note that long-term studies are needed.
How is restless legs syndrome treated?
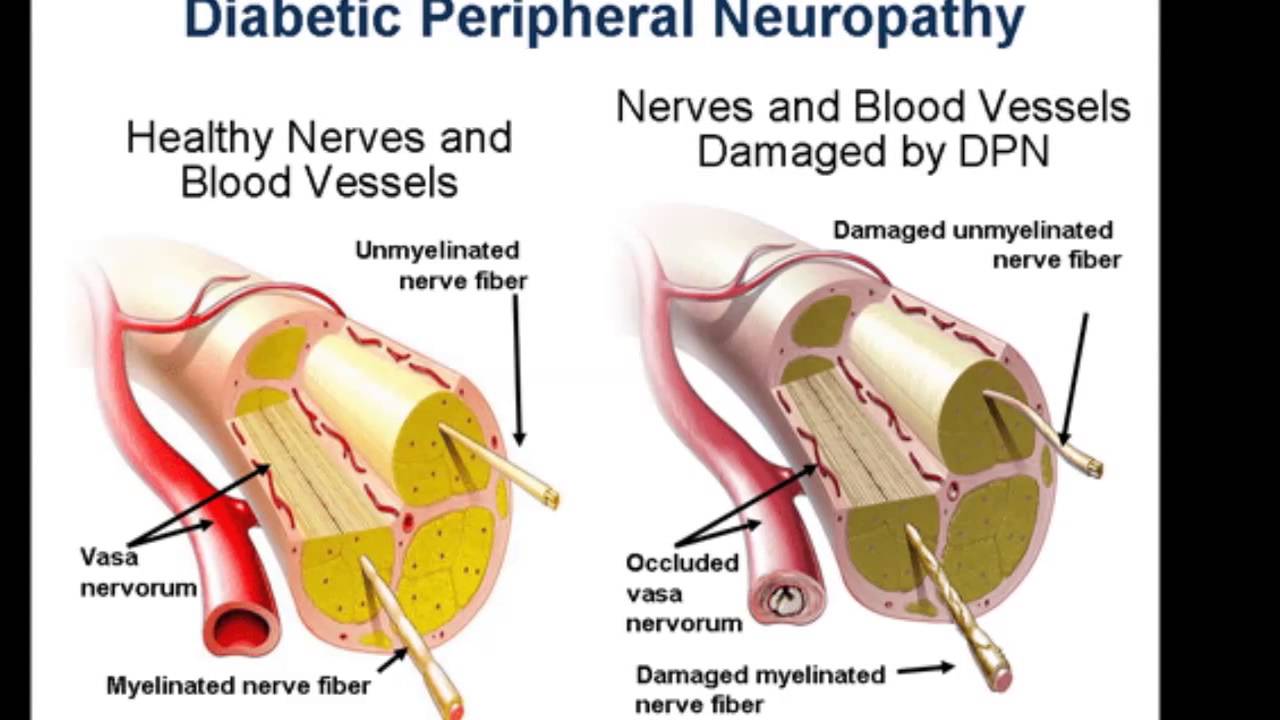
RLS can be treated, with care directed toward relieving symptoms. Moving the affected limb(s) may provide temporary relief. Sometimes RLS symptoms can be controlled by finding and treating an associated medical condition, such as peripheral neuropathy, diabetes, or iron deficiency anemia.
Iron supplementation or medications are usually helpful but no single medication effectively manages RLS for all individuals. Trials of different drugs may be necessary. In addition, medications taken regularly may lose their effect over time or even make the condition worse, making it necessary to change medications.
Treatment options for RLS include:
Lifestyle changes. Certain lifestyle changes and activities may provide some relief in persons with mild to moderate symptoms of RLS. These steps include avoiding or decreasing the use of alcohol and tobacco, changing or maintaining a regular sleep pattern, a program of moderate exercise, and massaging the legs, taking a warm bath, or using a heating pad or ice pack. There are new medical devices that have been cleared by the U.S. Food & Drug Administration (FDA), including a foot wrap that puts pressure underneath the foot and another that is a pad that delivers vibration to the back of the legs. Aerobic and leg-stretching exercises of moderate intensity also may provide some relief from mild symptoms.
Iron. For individuals with low or low-normal blood tests called ferritin and transferrin saturation, a trial of iron supplements is recommended as the first treatment. Iron supplements are available over-the-counter. A common side effect is upset stomach, which may improve with use of a different type of iron supplement. Because iron is not well-absorbed into the body by the gut, it may cause constipation that can be treated with a stool softeners such as polyethylene glycol. In some people, iron supplementation does not improve a person’s iron levels. Others may require iron given through an IV line in order to boost the iron levels and relieve symptoms.
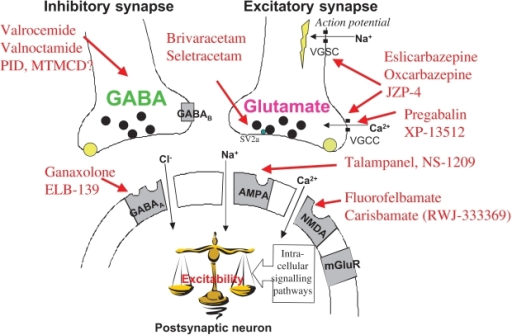
Anti-seizure drugs. Anti-seizure drugs are becoming the first-line prescription drugs for those with RLS. The FDA has approved gabapentin enacarbil for the treatment of moderate to severe RLS, This drug appears to be as effective as dopaminergic treatment (discussed below) and, at least to date, there have been no reports of problems with a progressive worsening of symptoms due to medication (called augmentation). Other medications may be prescribed “off-label” to relieve some of the symptoms of the disorder.
Other anti-seizure drugs such as the standard form of gabapentin and pregabalin can decrease such sensory disturbances as creeping and crawling as well as nerve pain. Dizziness, fatigue, and sleepiness are among the possible side effects. Recent studies have shown that pregabalin is as effective for RLS treatment as the dopaminergic drug pramipexole, suggesting this class of drug offers equivalent benefits.
Dopaminergic agents. These drugs, which increase dopamine effect, are largely used to treat Parkinson’s disease. They have been shown to reduce symptoms of RLS when they are taken at nighttime. The FDA has approved ropinirole, pramipexole, and rotigotine to treat moderate to severe RLS. These drugs are generally well tolerated but can cause nausea, dizziness, or other short-term side effects. Levodopa plus carbidopa may be effective when used intermittently, but not daily.
Although dopamine-related medications are effective in managing RLS symptoms, long-term use can lead to worsening of the symptoms in many individuals. With chronic use, a person may begin to experience symptoms earlier in the evening or even earlier until the symptoms are present around the clock. Over time, the initial evening or bedtime dose can become less effective, the symptoms at night become more intense, and symptoms could begin to affect the arms or trunk. Fortunately, this apparent progression can be reversed by removing the person from all dopamine-related medications.
Another important adverse effect of dopamine medications that occurs in some people is the development of impulsive or obsessive behaviors such as obsessive gambling or shopping. Should they occur, these behaviors can be improved or reversed by stopping the medication.
Opioids. Drugs such as methadone, codeine, hydrocodone, or oxycodone are sometimes prescribed to treat individuals with more severe symptoms of RLS who did not respond well to other medications. Side effects include constipation, dizziness, nausea, exacerbation of sleep apnea, and the risk of addiction; however, very low doses are often effective in controlling symptoms of RLS.
Benzodiazepines. These drugs can help individuals obtain a more restful sleep. However, even if taken only at bedtime they can sometimes cause daytime sleepiness, reduce energy, and affect concentration. Benzodiazepines such as clonazepam and lorazepam are generally prescribed to treat anxiety, muscle spasms, and insomnia. Because these drugs also may induce or aggravate sleep apnea in some cases, they should not be used in people with this condition. These are last-line drugs due to their side effects.