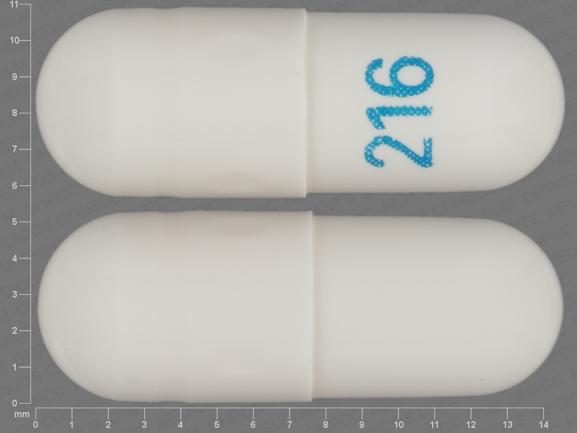
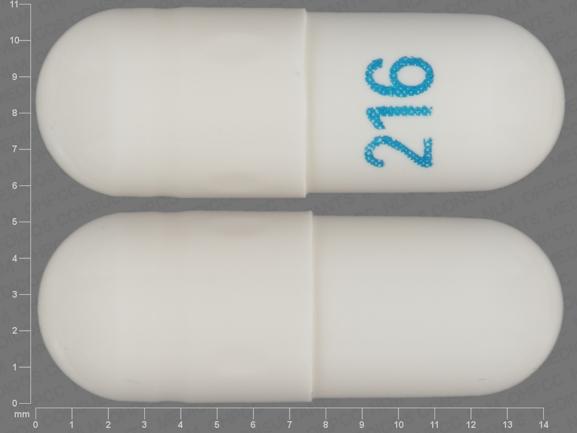
Pill with imprint 216 is White, Capsule/Oblong and has been identified as Gabapentin 100 mg. It is supplied by Ascend Laboratories, LLC.
Gabapentin is used in the treatment of Back Pain; Postherpetic Neuralgia; Epilepsy; Chronic Pain; Seizures and belongs to the drug class gamma-aminobutyric acid analogs. Risk cannot be ruled out during pregnancy. Gabapentin 100 mg is not a controlled substance under the Controlled Substances Act (CSA).
Gabapentin
- Imprint
- 216
- Strength
- 100 mg
- Color
- White
- Size
- 14.00 mm
- Shape
- Capsule/Oblong
- Availability
- Prescription only
- Drug Class
- Gamma-aminobutyric acid analogs
- Pregnancy Category
- C – Risk cannot be ruled out
- CSA Schedule
- Not a controlled drug
- Labeler / Supplier
- Ascend Laboratories, LLC
- Inactive Ingredients
- corn starch, lactose anhydrous, magnesium silicate, gelatin, sodium lauryl sulfate, titanium dioxide
Note: Inactive ingredients may vary.
Labelers / Repackagers
| NDC Code | Labeler / Repackager |
|---|---|
| 67877-0222 | Ascend Laboratories LLC |
| 16714-0503 | NorthStar Rx LLC |
What Is Gabapentin and What I should Know Before I Buy Gabapentin Online ?
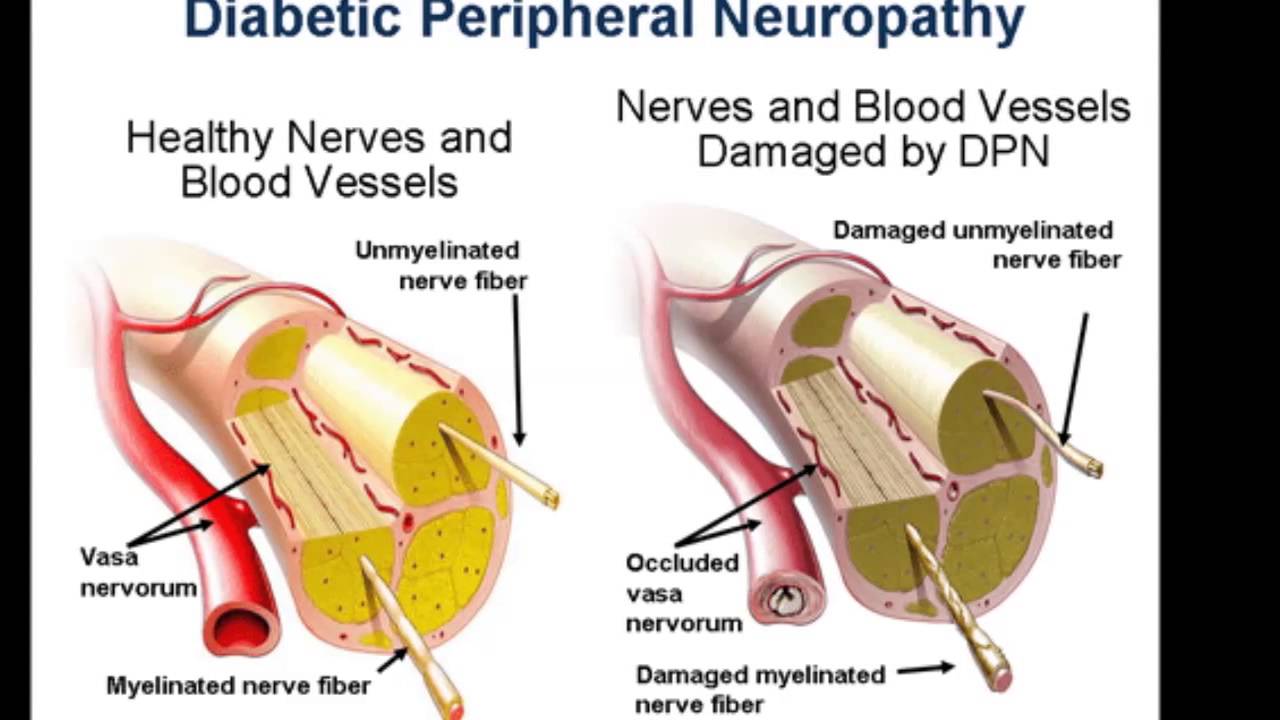
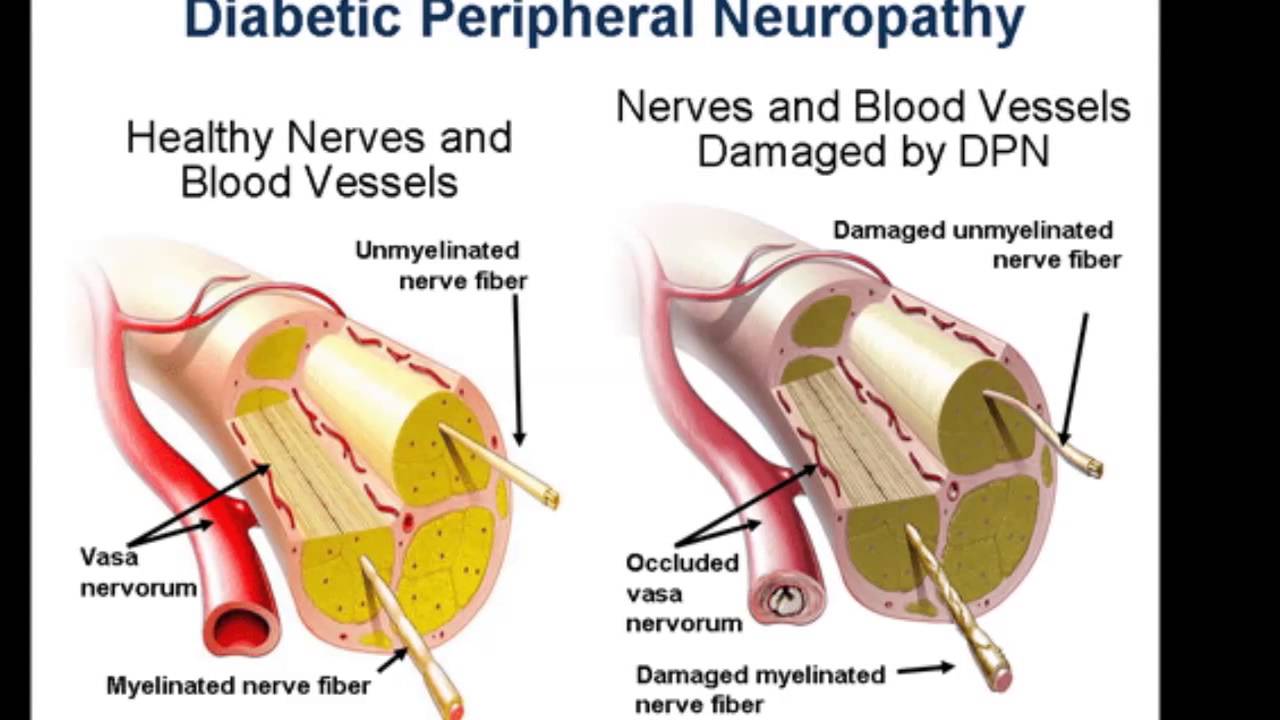
Gabapentin is a prescription medication primarily used to treat epilepsy, neuropathic pain, and restless legs syndrome (RLS). It belongs to a class of drugs known as anticonvulsants. Here’s a more detailed look at its uses and mechanisms:
- Uses:
- Seizure Management: Gabapentin is used as an adjunctive therapy to reduce the frequency of partial-onset seizures in adults and children aged three and older.
- Neuropathic Pain: It is commonly prescribed for the management of neuropathic pain, such as postherpetic neuralgia (pain following shingles).
- Restless Legs Syndrome (RLS): Gabapentin enacarbil, a prodrug of gabapentin (brand name Horizant), is used to treat moderate-to-severe RLS.
- Off-Label Uses: Gabapentin may also be used off-label for conditions like fibromyalgia, persistent hiccups, migraine prevention, and hot flashes.
- Mechanism of Action:
- While the exact mechanism is not fully understood, gabapentin is thought to work by modulating the activity of certain neurotransmitters in the brain and affecting the way the nervous system transmits pain signals.
What You Should Know Before Buying Gabapentin Online
- Prescription Requirement:
- Gabapentin is a prescription medication, meaning it legally requires a doctor’s prescription. Always ensure you have a valid prescription before purchasing it online.
- Source Legitimacy:
- Only buy gabapentin from reputable online pharmacies. Verify that the pharmacy is licensed and requires a prescription for purchase. Look for certifications like the Verified Internet Pharmacy Practice Sites (VIPPS) seal in the U.S.
- Potential Risks:
- Side Effects: Common side effects include dizziness, drowsiness, tiredness, fever, and nystagmus (rapid, uncontrollable eye movements). Gabapentin can also cause behavioral changes in children, blurred vision, dry mouth, peripheral edema, tremor, and gastrointestinal disturbances.
- Mental Health Risks: Gabapentin may increase the risk of depression and suicidal thoughts, particularly in young adults under 24 years old.
- Withdrawal Symptoms: Abruptly stopping gabapentin can lead to withdrawal symptoms such as anxiety, insomnia, nausea, pain, and sweating. It should be tapered off slowly under a doctor’s guidance.
- Drug Interactions: Gabapentin can interact with other medications, including antacids, hydrocodone, morphine, and other drugs that cause sedation or dizziness. It may also cause false-positive results on some urinary protein tests.
- Dosage Adjustments:
- The dosage of gabapentin needs to be adjusted for individuals with kidney disease. Always follow your doctor’s instructions regarding dosage.
- Quality and Authenticity:
- Be cautious of counterfeit medications. Authentic gabapentin should come from a reliable source, and the packaging should be intact with proper labeling.
- Misuse and Abuse Potential:
- Gabapentin has been associated with misuse and abuse, particularly in individuals with a history of drug abuse. Be mindful of this potential and use the medication only as prescribed.
- Cost and Insurance:
- Check if the online pharmacy accepts your insurance or offers competitive pricing. Compare prices from different legitimate sources to ensure you are getting a fair deal.
Ascend Laboratories
Ascend Laboratories is a pharmaceutical company that specializes in the development, manufacturing, and distribution of generic pharmaceuticals. Ascend Laboratories, as a subsidiary of Alkem Laboratories, plays a significant role in the generic pharmaceutical industry. With a strong focus on quality, regulatory compliance, and affordability, Ascend Laboratories continues to expand its presence in the U.S. market. The company’s commitment to sustainable practices and community engagement further underscores its dedication to improving healthcare access and quality of life for patients.
Here is an overview of Ascend Laboratories:
Company Overview
- Headquarters:
- Location: Montvale, New Jersey, USA.
- Parent Company:
- Alkem Laboratories: Ascend Laboratories is a wholly-owned subsidiary of Alkem Laboratories, a leading Indian pharmaceutical company that is known for its wide range of generic medicines and active pharmaceutical ingredients (APIs).
Operations and Facilities
- Manufacturing:
- Ascend Laboratories benefits from the extensive manufacturing network of Alkem Laboratories, which includes facilities in India and the United States. These facilities are designed to meet stringent regulatory standards set by agencies like the U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), and other global health authorities.
- Product Development:
- The company focuses on developing high-quality generic medications across various therapeutic areas. The product development process involves rigorous research, formulation, and testing to ensure that the generics are bioequivalent to their branded counterparts.
Product Portfolio
- Generics:
- Ascend Laboratories offers a broad range of generic pharmaceuticals covering multiple therapeutic categories, including cardiovascular, central nervous system, anti-infective, gastrointestinal, and pain management drugs.
- The company’s products are known for their affordability and quality, making essential medications accessible to a wider patient population.
- OTC Products:
- In addition to prescription medications, Ascend Laboratories also offers over-the-counter (OTC) products that address common health concerns.
Key Areas of Operation
- Regulatory Compliance:
- Quality Assurance: Ascend Laboratories adheres to rigorous quality control measures and regulatory requirements to ensure the safety, efficacy, and quality of its products.
- GMP Compliance: The company’s manufacturing processes comply with Good Manufacturing Practices (GMP), ensuring that all products meet high standards of quality.
- Market Strategy:
- Product Launches: The company focuses on the timely introduction of generic medications to the market, providing affordable options as patents for branded drugs expire.
- Competitive Pricing: Ascend’s pricing strategy ensures that its products remain affordable without compromising on quality.
- Distribution Networks:
- Ascend Laboratories has established robust distribution networks that ensure the widespread availability of its products across the United States.
Strategic Growth
- Acquisitions and Partnerships:
- Ascend Laboratories leverages the global presence and expertise of Alkem Laboratories to expand its market reach through strategic acquisitions and partnerships.
- The company continuously seeks opportunities to enhance its product portfolio and enter new markets.
- Innovation:
- The company is committed to innovation in generic pharmaceuticals, focusing on developing complex generics and novel drug delivery systems to address unmet medical needs.
Corporate Responsibility
- Sustainability:
- Ascend Laboratories is committed to sustainable business practices, including minimizing environmental impact through efficient resource use and waste management.
- Community Engagement:
- The company engages in corporate social responsibility (CSR) initiatives aimed at improving healthcare access, supporting education, and contributing to the well-being of the communities it serves.
I Want to Buy Gabapentin, What Should I know Before I see A doctor ?
If you’re considering gabapentin, it’s important to consult with a doctor beforehand. Here are some key points to consider before your appointment:
- Medical History: Be prepared to discuss your medical history with your doctor, including any past or current conditions, medications you’re taking, and any allergies you may have.
- Reason for Use: Be ready to explain why you believe gabapentin may be necessary for your health. Whether it’s for epilepsy, neuropathic pain, or another condition, your doctor will need to understand your symptoms and medical needs.
- Potential Side Effects: Familiarize yourself with the potential side effects of gabapentin. These can include dizziness, drowsiness, and coordination problems. Understanding the possible risks can help you make an informed decision.
- Interactions: Gabapentin can interact with other medications, including over-the-counter drugs and supplements. Make sure to inform your doctor of all medications you’re taking to avoid any potential interactions.
- Dosage and Administration: Your doctor will determine the appropriate dosage of gabapentin based on your condition and medical history. Be prepared to discuss dosing instructions and how to take the medication correctly.
- Monitoring: Your doctor may recommend regular check-ups to monitor your progress and adjust your treatment plan if necessary. It’s important to follow up with your doctor as directed to ensure the medication is working effectively and safely.
- Pregnancy and Breastfeeding: If you are pregnant, planning to become pregnant, or breastfeeding, discuss this with your doctor. Gabapentin may not be suitable during pregnancy or while breastfeeding, and your doctor can advise you on the best course of action.
- Alternative Treatments: Explore alternative treatments or therapies that may be available for your condition. Your doctor can help you weigh the benefits and risks of gabapentin compared to other options.
By discussing these points with your doctor, you can ensure that gabapentin is the right choice for you and that you understand how to use it safely and effectively.