In a meta-analysis of trials evaluating the treatment of neuropathic pain, including painful polyneuropathy and spinal cord injury pain, gabapentin was shown to be safe and effective .
Data from meta-analyses support the use of immediate-release gabapentin for reducing pain by more than 50% in diabetic neuropathy.
Data from a limited number of clinical trials support the use of extended-release gabapentin in reducing pain by more than 50% and improving sleep in diabetic neuropathy.
Gabapentin (Neurontin) has FDA indication to treat postherpetic neuralgia and partial onset seizures. Controlled clinical trials in diabetic neuropathy and postherpetic neuralgia show that gabapentin at 2400-3600 mg/day has a similar efficacy to tricyclic antidepressants and carbamazepine. Consistent, though less compelling clinical evidence supports its use for neuropathic cancer pain, pain associated with HIV infection, chronic back pain and others (readers wanting more in depth research findings are urged to consult Reference 1).
Due to this emerging evidence, it is widely used for the treatment of neuropathic pain. The exact mechanism and site of action of gabapentin is unknown. Gabapentin is generally well-tolerated, easily titrated, has few drug interactions, and does not require laboratory monitoring. However, cost may be a limiting factor for some patients.
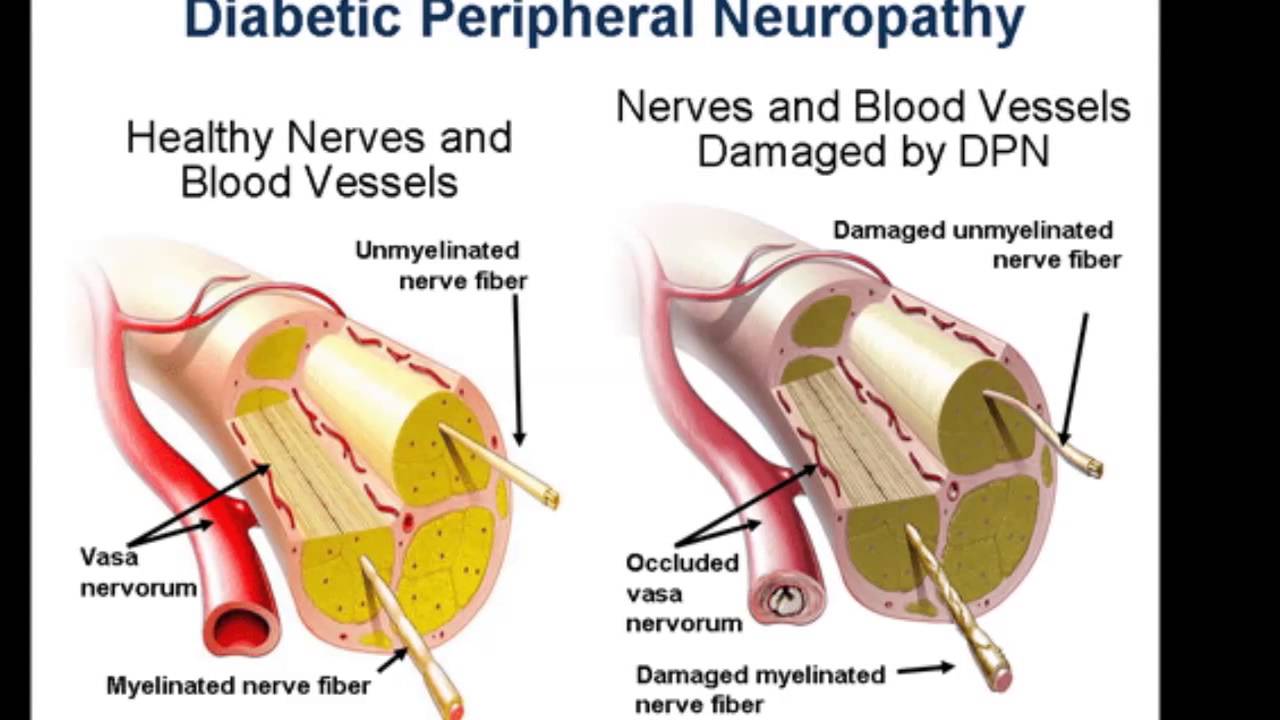
Patients suitable for gabapentin should have a clear neuropathic pain syndrome, characterized by sharp, shooting, lancinating and/or burning pain, in a nerve root (radicular) or stocking/glove distribution. See Fast Fact #289 for a comparison of gabapentin with pregabalin a similar neuropathic analgesic.
Adult Dosing Gabapentin is started at low doses (100 mg to 300 mg total daily) and increased by 100 – 300 mg every 1-3 days to effect. A typical schedule might be: day 1-2: 300 mg nightly; day 3-4: 300 mg twice daily; day 5-7: 600 mg twice daily; day 8 onwards: 600 mg three times a day. The usual effective total daily dose is 900-3600 mg, administered in three divided doses per day. Titration should proceed more slowly in elderly patients. If gabapentin is discontinued, it should be done over a minimum of a week to prevent withdrawal seizures.
Pediatric Use There is limited data available assessing its effectiveness in neuropathic pain in children. The American Pain Society recommends that gabapentin be considered for pediatric neuropathic pain especially when concurrent analgesics are found to be too sedating. Their recommended initial dose is 2 mg/kg/day with a usual dosage range of 8 to 35 mg/kg/day divided into 3 daily doses.
Dosing in Renal Failure Gabapentin doses must be reduced for patients with renal insufficiency.
- Creatinine Clearance (CrCl) 30-60 ml/min: maximum daily dose is 1400 mg, divided.
- CrCl 16-30 ml/min: maximum daily dose is 700 mg, given once daily.
- CrCl 15ml/min: maximum daily dose is 300 mg, once daily. Doses should decrease proportionally for CrCl less than 15 ml/min (e.g. 300 mg every other day for a CrCl of ~7.5 ml/min).
- For patients on hemodialysis a supplemental dose is usually given after dialysis (usually 100-300 mg).
Adverse Reactions Sedation, confusion, dizziness, and ataxia are the most common side effects, especially with rapid dose titration. Tolerance to these effects appears to develop within a few days if the dose is held at the highest tolerated dose until symptoms improve or stabilize.
Dosage Formulations Gabapentin is available in 100 mg, 300 mg, and 400 mg capsules, 600 mg and 800 mg tablets, and as a liquid (250mg/5mL).
Cost Gabapentin is more expensive than older agents used for neuropathic pain (tricyclic antidepressants and older anti-epileptic drugs such as carbamazepine). Generic gabapentin is available, although can cost ~$100 for 90 600 mg tablets.
Other Palliative Care Uses of Gabapentin Small scale published trials have shown efficacy in the treatment of severe chronic hiccups, pruritus, postoperative pain and delirium, restless leg syndrome and hot flashes. Perhaps more compelling is its potential efficacy for chronic cough for which a randomized double-blind placebo controlled trial demonstrated significant improvement in cough-specific quality of life, cough frequency, and cough severity. See Fast Fact #200.
Summary Gabapentin is a safe and effective adjuvant analgesic for neuropathic pain. Physicians should become comfortable using and titrating gabapentin in patients with neuropathic pain syndromes.
Based on guidelines from the International Association for the Study of Pain (IASP), European Federation of Neurological Societies (EFNS), and Society of Critical Care Medicine (SCCM), gabapentin is effective and recommended for the management of peripheral neuropathy .
Based on guidelines from the EFNS, IASP, and National Institute for Health and Care Excellence (NICE), gabapentin is effective and recommended as first-line therapy, supported by strong evidence, in the management of diabetic neuropathy.
The IASP guidelines recommend both immediate- and extended-release gabapentin . In contrast, a guideline from the American Academy of Neurology (AAN), American Association of Neuromuscular and Electrodiagnostic Medicine, and American Academy of Physical Medicine and Rehabilitation states that gabapentin is probably effective and should be considered an alternative treatment for painful diabetic neuropathy based on limited benefit in 2 controlled trials.
Similarly, a position statement from the American Diabetes Association (ADA) recommends gabapentin as a second-line option .
